Cheat Sheets and Downloads
Split/Shared Substantive Portion Audit Checklist
The 2025 Medicare rule defining the "Substantive Portion" for Split/Shared visits is no longer theoretical—it's actively costing health systems revenue. If physician documentation doesn't clearly assign the substantive portion via Time or Medical Decision Making (MDM), the entire visit is defaulted to the NPP rate, resulting in a 15% cut to reimbursement and a direct loss of physician wRVUs. Don't wait for the audit findings.
Cath‑Lab Teams: 2025 Regulatory Overhaul is Here

Is your cath lab ready for the seismic shifts ahead?
These five focus areas will impact revenue, coding, and compliance in 2025:
🧠 Use G0537/G0538 for ASCVD risk-based reimbursement
✅ Ensure quality reporting to unlock OPPS increases
📋 Adapt to HCC v28 with granular documentation
🔍 Audit modifiers to prevent denials
Case Studies
Revenue Recovery Through Proper Split/Shared Visit Documentation

The Challenge: A Physician Retention Crisis
A top Cardiothoracic Surgery practice faced a crisis when its two surgeons, highly dissatisfied with their pay, threatened to quit. An internal review exposed the cause: their outsourced Revenue Cycle Management (RCM) company was systematically under-billing their work. The core issue was the misapplication of Medicare rules for visits involving Advanced Practice Providers (APPs), causing substantial loss of revenue and physician compensation based on work RVUs.

The Critical Finding: Lost Revenue from Incorrect Coding
An emergency audit revealed two major systematic errors. The RCM company was incorrectly billing physician-attested office visits as split/shared at the reduced 85% APP rate, instead of the full Incident-to rate. Furthermore, the physicians' hospital documentation was inadequate for them to be the billing provider. These errors led to an estimated loss of over $\$220,000$ in annual revenue and directly reduced the surgeons' compensation by $\$54,000$ per year.

The Solution: Oversight and Policy Correction
We implemented a phased solution focused on correcting policy and establishing physician oversight. This involved re-training the RCM team on the fundamental difference between Office Incident-to and Hospital Split/Shared rules. We also created new documentation templates to ensure physicians properly captured their work in hospital settings. A key outcome was the establishment of surgeon involvement in billing policy, shifting away from the unsupervised outsourced model.

The Results: Full Financial and Talent Recovery
Within six months, the practice achieved full financial correction. We successfully recovered the lost revenue, which was subsequently annualized at $\$222,492$. Crucially, the surgeons received true-up payments to correct past under-compensation, leading them to withdraw their resignation threats and sign long-term contract extensions. This case demonstrates the critical need for internal oversight of outsourced RCM and the direct link between proper billing and physician satisfaction.
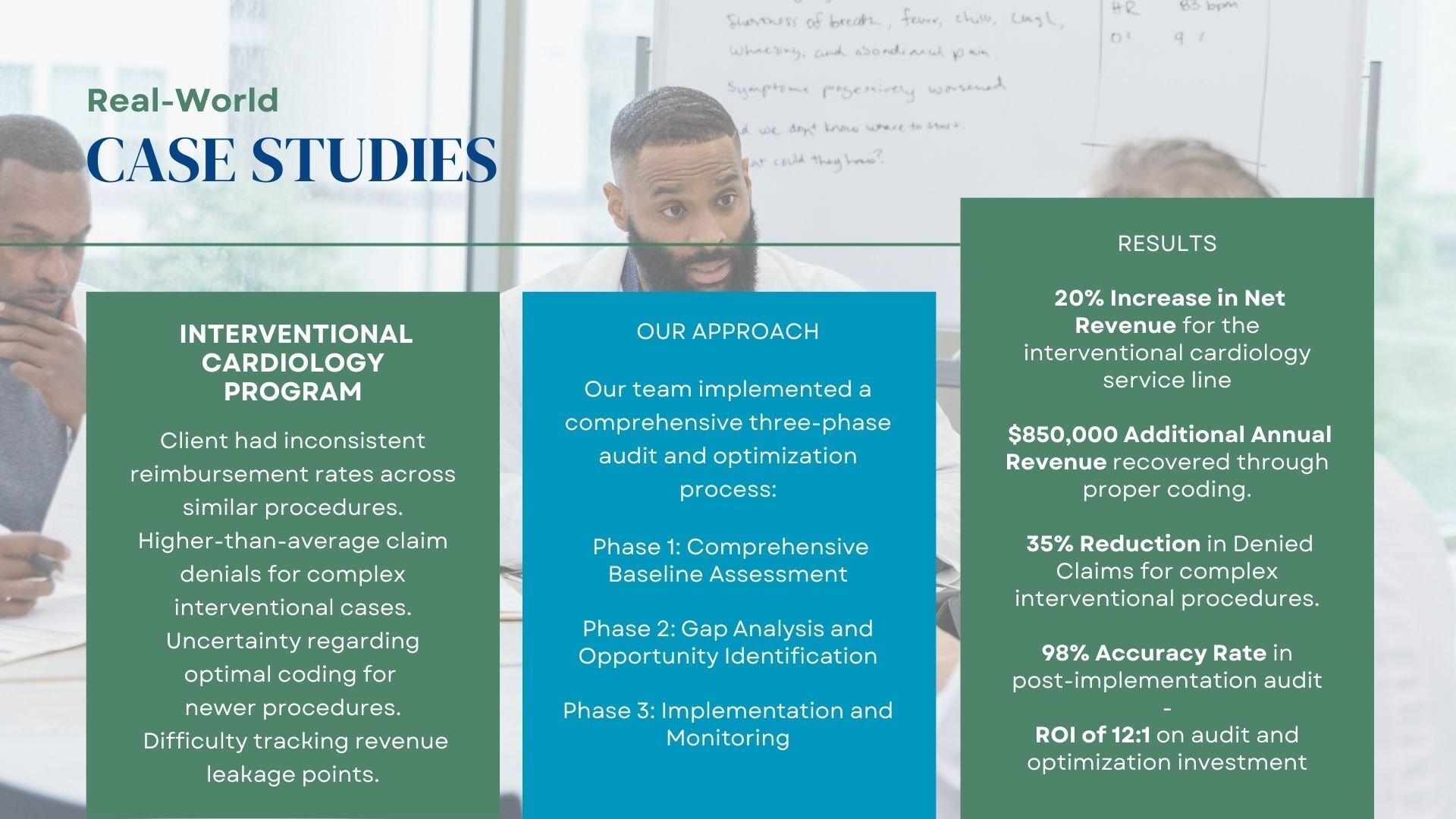
Interventional Cardiology Program
Our export team is familiar with recent changes to Cath Lab billing requirements. Our team will with start with an assessment. Identify any gaps and opportunities and implement ongoing best practices and monitoring to ensure reimbursement rates are accurate on complex claims. Learn more about recent Cath Lab changes by downloading our cheat sheet.